Healthcare Operations
COVID-19 Hospital Capacity Management using Mathematical Models
We use mathematical optimization to determine optimal strategies to reduce the burden of COVID-19 on hospitals. In particular, we focus on patient transfers. In practice, hospitals, even those in the same region or system, experience very different COVID patient loads, meaning that some may have unused capacity even while COVID overwhelms other hospitals. Patient transfers can balance these uneven loads and ensure that all capacity to care for patients is efficiently used. Patient transfers were used by some hospital systems that were hit particularly hard during the first wave of the pandemic, but these transfers were generally made reactively as hospitals ran out of capacity rather than planned. Optimal coordinated transfers have potential to significantly help hospitals cope with the burden of COVID and ensure that all patients receive the best possible level of care. We aim to demonstrate the benefits of this approach on this website using real-world data.
REAL-TIME SCHEDULING FOR OUTPATIENT CLINICS
EFFECTS OF STAFFING PATTERNS ON PATIENT CARE
LEVEL-LOADING IN PRIMARY CARE CLINICS
IMPROVING OPERATING ROOMS SCHEDULING UNDER UNCERTAINTY
AN INDUSTRY 4.0 APPROACH TO HEALTHCARE ENERGY SUSTAINABILITY
ENERGY ANALYSIS OF HEALTHCARE INFECTION CONTROL INTERVENTIONS WITHIN HOSPITALS FOR COVID-19
MINIMIZING SECONDARY INFECTIONS IN HOSPITALS

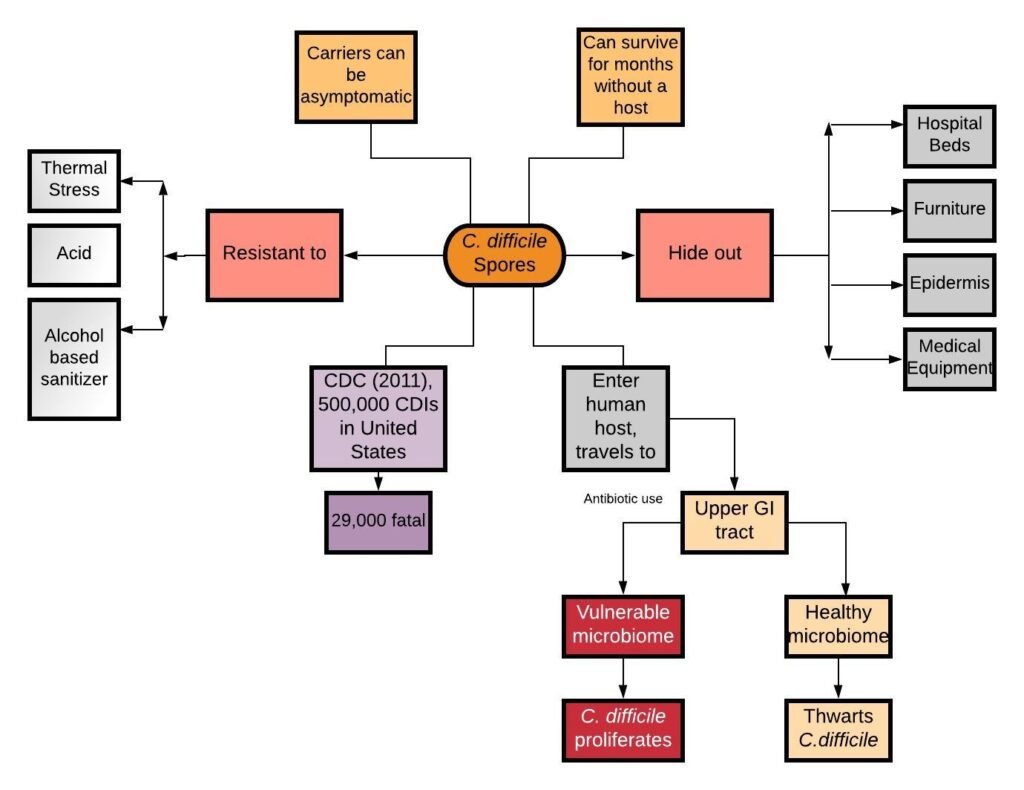
RISK CALCULATOR FOR C. DIFFICILE INFECTIONS AT THE HOSPITAL UNIT LEVEL